Overview
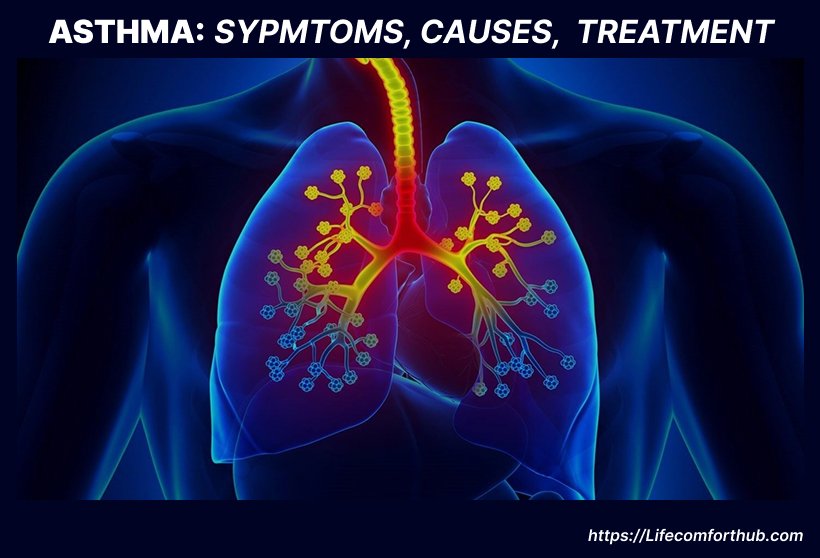
Asthma is a chronic respiratory condition that affects millions globally. While it cannot be cured, effective management can significantly improve quality of life. This article synthesizes information from reputable sources to provide a comprehensive overview of asthma, its symptoms, causes, diagnosis, treatment, and prevention strategies.
Contents
Introduction to Asthma | Symptoms of Asthma | Causes of Asthma | Diagnosis of Asthma | Treatment of Asthma | Prevention of Asthma
Introduction to Asthma
What Is Asthma?
Asthma is a long-term, chronic disease that affects the lungs by causing inflammation and narrowing of the airways. This makes it difficult to breathe and can lead to coughing, wheezing, chest tightness, shortness of breath, and excess mucus production.
For some people, asthma is mild and manageable. For others, it can significantly interfere with daily life or lead to life-threatening attacks. An asthma attack happens when symptoms suddenly worsen due to tightened airway muscles (bronchospasm), swelling, and increased mucus. This limits airflow and can prevent enough oxygen from reaching the lungs and bloodstream.
Asthma affects more than 25 million people in the United States, including over 5 million children. It’s the most common chronic lung condition among kids and a leading cause of emergency room visits.
While asthma can’t be cured, it can be effectively managed with the right treatment. This usually involves medications, lifestyle adjustments, and working closely with a healthcare provider to track symptoms and make treatment changes as needed.
Types of Asthma
What are the types of Asthma
There are many different types of asthma, but i will classifying them by their symptom patterns, Cause or trigger, Age of Onset, Special or Severe forms.
Symptom Pattern
-
Intermittent Asthma
Symptoms come and go. You may feel fine between episodes. Flare-ups are usually triggered by specific exposures or activities. -
Persistent Asthma
Symptoms occur more regularly—daily or weekly—and can be mild, moderate, or severe. Persistent asthma can interfere with sleep, work, and physical activity.
Cause or Trigger
-
Allergic Asthma
Triggered by allergens like pollen, mold, pet dander, or dust mites. This is the most common type and often overlaps with seasonal allergies. -
Non-Allergic Asthma
Triggered by irritants not related to allergies, such as cold air, smoke, air pollution, strong smells, or viral infections. -
Exercise-Induced Bronchoconstriction (EIB)
Narrowing of the airways during or after physical activity. It can occur in people with or without other forms of asthma. -
Occupational Asthma
Caused by exposure to substances at work—such as dust, chemicals, fumes, or animal proteins. Common in farming, manufacturing, and textile industries. -
Aspirin-Induced Asthma (AIA)
Triggered by aspirin or NSAIDs like ibuprofen. Usually occurs in adults and may be associated with nasal polyps and sinus issues. -
Nocturnal Asthma
Symptoms worsen at night, often disrupting sleep. Triggers can include allergens, reflux, or natural changes in airway function during sleep. -
Seasonal Asthma
Triggered by environmental factors that appear at certain times of the year—such as pollen in spring or cold air in winter. -
Cough-Variant Asthma (CVA)
The main symptom is a chronic, dry cough. It often lacks the typical wheezing and breathlessness seen in other types.
Age of Onset
-
Pediatric (Childhood) Asthma
Often starts before age 5. Common triggers include viral infections, allergens, and smoke. Some children outgrow it, while others continue into adulthood. -
Adult-Onset Asthma
Begins after age 18. May be harder to diagnose due to overlapping conditions. Triggers include respiratory illness, allergies, stress, or workplace irritants.
Special or Severe Forms
-
Eosinophilic Asthma
A severe, treatment-resistant form marked by high levels of eosinophils (a type of white blood cell). Usually affects adults and may require advanced therapies. -
Status Asthmaticus
A prolonged asthma attack that doesn’t respond to standard treatments. This is a medical emergency requiring immediate care. -
Asthma-COPD Overlap Syndrome (ACOS)
A condition where a person shows features of both asthma and chronic obstructive pulmonary disease (COPD). Symptoms are more severe and harder to control. -
Difficult-to-Control or Severe Refractory Asthma
Asthma that remains poorly controlled despite high doses of medication and correct inhaler use. May require specialist care and biologic therapy.
Symptoms of Asthma
Asthma presents with a range of respiratory symptoms that can vary in intensity, frequency, and duration. Some individuals experience occasional, mild symptoms, while others have chronic or severe manifestations that interfere with daily life.
Common Symptoms
-
Shortness of breath
-
Chest tightness or discomfort
-
Wheezing (especially during exhalation)
-
Coughing, particularly at night or early morning
-
Difficulty sleeping due to breathing issues
These symptoms result from airway inflammation, bronchial constriction, and excess mucus production. Wheezing is a hallmark finding, especially in children, but it may not be present in all cases. Nighttime symptoms are common and often disrupt sleep, leading to daytime fatigue.
Early Warning Signs
-
Increased coughing, especially at night
-
Fatigue or reduced tolerance to physical activity
-
Mild breathlessness during normal exertion
-
Mood changes such as irritability or restlessness
-
Drop in peak flow readings
These early signs can appear hours or even days before a noticeable exacerbation. Recognizing and responding to them—by adjusting medications or following an action plan—can help prevent a full-blown attack.
Exacerbation Symptoms (Flare-ups)
-
Persistent wheezing and coughing
-
Rapid or labored breathing
-
Chest pain or pressure
-
Use of accessory muscles to breathe
-
Difficulty speaking in full sentences
-
Anxiety or panic
-
Cyanosis (bluish lips or fingertips in severe cases)
An exacerbation, or asthma attack, occurs when the airways become severely narrowed. Mucosal swelling, bronchospasm, and increased mucus obstruct airflow, making breathing progressively more difficult. Severe cases require immediate medical intervention to restore airway function.
Atypical Presentations
-
Chronic dry cough without wheezing (cough-variant asthma)
-
Frequent throat clearing or sighing
-
Sleep disturbances without obvious cause
-
Exercise intolerance in the absence of other symptoms
These less common symptoms can lead to delayed diagnosis or misdiagnosis. It’s important to consider these presentations, especially when evaluating unexplained respiratory complaints in both adults and children.
When to Seek Immediate Medical Attention
-
Severe shortness of breath or gasping for air
-
Inability to speak or walk due to breathing difficulty
-
Lack of response to quick-relief medication
-
Bluish discoloration of lips or nails
-
Peak flow less than 50% of personal best
These are signs of a medical emergency. Without prompt treatment, oxygen levels can fall to dangerous levels, resulting in loss of consciousness or death.
Causes of Asthma
What are the Causes and Triggers
The precise cause of asthma remains unclear, but current evidence suggests a multifactorial origin involving genetic predisposition, environmental exposures, immune system development, and other modifying factors. While the underlying causes set the foundation for the disease, specific triggers often provoke or worsen symptoms.
Underlying Causes
Genetics
A family history of asthma, allergic rhinitis, eczema, or other atopic conditions significantly increases the likelihood of developing the disease. Individuals with one or both parents affected are at particularly elevated risk, indicating a strong hereditary component.
Allergic Sensitization
Allergies play a central role in many cases. Exposure to allergens such as pollen, dust mites, pet dander, or mold can initiate immune responses that contribute to chronic airway inflammation. Allergic asthma is the most common subtype and frequently coexists with other allergic conditions like hay fever or food allergies.
Early-Life Respiratory Infections
Severe viral infections in infancy or early childhood—especially those involving respiratory syncytial virus (RSV) or bronchiolitis—can impair lung development and immune regulation, increasing susceptibility later in life.
Hygiene Hypothesis
Limited microbial exposure in early childhood may lead to an under-stimulated immune system that becomes overly reactive to harmless substances. This theory is supported by data showing lower asthma rates in children exposed to farm environments or those with older siblings.
Environmental Exposures in Early Life
High exposure to cigarette smoke, indoor or outdoor pollutants, and airborne chemicals during critical periods of lung development may increase the risk of asthma onset, particularly in infants and young children.
Obesity
Excess body weight has been associated with increased disease risk and severity. Obesity may alter lung mechanics, increase systemic inflammation, and reduce response to standard therapies.
Hormonal Factors
Hormonal changes during menstruation, pregnancy, or menopause may influence symptoms. Some women experience symptom fluctuations tied to their menstrual cycle—a phenomenon known as perimenstrual asthma. Hormonal shifts may impact airway reactivity and inflammation.
Prematurity and Low Birth Weight
Children born prematurely or with low birth weight are at greater risk due to underdeveloped lungs and a potentially altered immune response.
Occupational Exposure
Repeated inhalation of certain workplace substances—such as chemical fumes, wood dust, latex, or cleaning agents—can lead to occupational asthma. This form often develops in adulthood and may persist even after the exposure ceases.
Common Triggers
Triggers are specific exposures or conditions that provoke symptoms in individuals with asthma. These vary widely between individuals and may evolve over time.
Allergens
Common allergens that act as triggers include:
-
Pollen
-
Mold spores
-
Dust mites
-
Pet dander
-
Cockroach waste
Even brief exposure to these allergens may cause inflammation and airway constriction in sensitized individuals.
Respiratory Infections
Upper respiratory tract infections, particularly viral illnesses such as the common cold or influenza, are a leading cause of symptom exacerbation. In children, asthma often becomes more apparent following such infections.
Exercise
Physical activity, especially in cold or dry air, can provoke airway narrowing. This is known as exercise-induced bronchoconstriction and is common even among individuals without chronic symptoms.
Environmental Irritants
Air pollution—including traffic emissions, industrial fumes, and wildfire smoke—can irritate the airways and precipitate flare-ups. Indoor pollutants, such as smoke from tobacco or wood-burning stoves, also pose significant risks.
Tobacco Smoke
Exposure to tobacco smoke, whether active or passive (secondhand), is a well-established trigger. Smoking also reduces the effectiveness of medications and contributes to disease progression.
Cold Air and Weather Changes
Sudden drops in temperature or inhaling cold, dry air can trigger symptoms by irritating airway linings and promoting bronchospasm.
Strong Odors and Chemicals
Perfumes, cleaning agents, paint fumes, and other volatile chemicals may act as irritants, particularly in individuals with heightened airway sensitivity.
Others are:
Certain Medications
Drugs such as nonsteroidal anti-inflammatory agents (e.g., ibuprofen, naproxen) and beta-blockers may exacerbate symptoms in some individuals. Aspirin-exacerbated respiratory disease (AERD) is a known subtype involving hypersensitivity to aspirin and related drugs.
Food Additives
Sulfites and preservatives found in processed foods—such as dried fruits, shrimp, and some wines—can trigger episodes in sensitive individuals.
Gastroesophageal Reflux Disease (GERD)
Reflux of stomach acid into the esophagus and airways can worsen respiratory symptoms. Managing GERD may improve asthma control in affected patients.
Pests
Exposure to cockroaches, mice, or other pests—often through their waste products—can worsen symptoms, especially in urban or poorly ventilated environments.
Intense Emotions
Episodes of laughter, crying, anger, or excitement can lead to hyperventilation and airway narrowing, triggering symptoms in some individuals.
Psychological Stress
Chronic or acute emotional stress may exacerbate symptoms or even contribute to disease development. Stress-related hormonal and immune responses are believed to influence airway sensitivity and inflammation.
Diagnosis of Asthma
Diagnosing asthma involves evaluating symptoms, ruling out other conditions, and confirming variable airway obstruction through objective testing.
Medical History and Physical Exam
A clinician will assess respiratory symptoms such as wheezing, coughing, and breathlessness, along with their frequency, triggers, and impact. Family history of asthma or allergies is also considered. During the physical exam, the provider listens for wheezing, checks nasal passages for inflammation, and examines the skin for signs of allergic conditions.
Lung Function Testing
Spirometry is the most common test, measuring how much and how quickly air can be exhaled. A bronchodilator may be used to see if airflow improves—an indicator of reversible obstruction. Peak flow monitoring may also be used to track lung performance over time.
Additional Tests
If standard tests are inconclusive, further evaluation may include:
-
Methacholine challenge to provoke airway narrowing
-
Exercise or cold-air provocation tests
-
Exhaled nitric oxide (FeNO) to detect airway inflammation
-
Sputum eosinophil count to assess allergic inflammation
Allergy Testing and Imaging
Skin or blood tests may identify allergic triggers. Chest X-rays are used to exclude other diagnoses.
Special Considerations
In young children who can’t perform lung function tests, diagnosis often relies on clinical history and response to treatment.
Asthma is typically diagnosed when symptoms improve with bronchodilators and other causes have been excluded.
Treatment of Asthma
The goal of asthma treatment is to manage symptoms, minimize flare-ups, and enhance overall quality of life. Treatments generally fall into two categories: quick-relief (rescue) medications and long-term control (maintenance) therapies.
Quick-relief medications are used during asthma episodes or for immediate symptom relief. The most commonly used are short-acting beta-agonists (SABAs) like albuterol, which work by rapidly relaxing airway muscles to ease breathing. In some emergency cases, anticholinergics such as ipratropium may also be administered.
Long-term control medications are taken daily to keep symptoms at bay and manage inflammation. Inhaled corticosteroids, like fluticasone and budesonide, are the most effective for long-term use, as they help to calm airway inflammation. Long-acting beta-agonists (LABAs), such as salmeterol, are often used in combination with corticosteroids in a single inhaler, providing both anti-inflammatory and bronchodilating effects.
Additional long-term options include leukotriene modifiers like montelukast, which target inflammation-causing chemicals, and theophylline, a bronchodilator that is less commonly prescribed. For more severe asthma, biologic therapies such as omalizumab or dupilumab are available and work by targeting specific immune system responses.
People with allergy-related asthma may benefit from allergy-specific treatments, including immunotherapy (allergy shots) or antihistamines.
Lifestyle adjustments are equally important. Avoiding known triggers such as smoke, dust, and allergens, using air purifiers, and sticking to a personalized asthma action plan are essential strategies. Regular doctor visits help assess lung function and make necessary adjustments to the treatment plan.
In serious asthma flare-ups, oral or intravenous corticosteroids may be used to swiftly reduce inflammation.
Prevention of Asthma
If you have asthma, you can’t prevent the condition itself, but you can prevent attacks by avoiding triggers and managing your health.
To reduce asthma attacks:
-
Avoid known triggers like smoke, chemicals, or allergens (e.g., dust, mold).
-
Take preventive meds as prescribed and follow your asthma action plan.
-
Consider allergy shots if allergies are a major trigger.
Daily habits that help:
-
Eat a healthy diet and avoid food allergens.
-
Maintain a healthy weight.
-
Quit smoking.
-
Exercise regularly (with your doctor’s guidance).
-
Manage stress.
With the right care and habits, asthma can be well controlled.
Sources
-
American Lung Association
https://www.lung.org/lung-health-diseases/lung-disease-lookup/asth/managing-asth -
National Heart, Lung, and Blood Institute (NHLBI)
https://www.nhlbi.nih.gov/health/asth -
Allergy & Asthma Network
https://allergyasthmanetwork.org/what-is-asth/lifestyle-changes-to-manage-asth/ -
Environmental Protection Agency (EPA)
https://www.epa.gov/asthma/asth-triggers-gain-control -
Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/asthma/expert-answers/asth-diet/faq-20058105 -
Healthline
https://www.healthline.com/health/asth -
WebMD
https://www.webmd.com/asthma/ss/slideshow-asth-and-your-diet - NHS.uk
https://www.nhs.uk/conditions/asth/ - Medical News Today
https://www.medicalnewstoday.com/articles/323523
Don’t self prescribe ensure to contact your Doctor before taking any medication.
Read more @ https://lifecomforthub.com/